Post-SSRI sexual dysfunction
Post-SSRI sexual dysfunction (PSSD),[1][2][3][4] also known as post-SSRI syndrome,[5] is a disorder in which people who have taken selective serotonin reuptake inhibitors (SSRIs) or other serotonin reuptake-inhibiting (SRI) drugs report persistent changes in sexual function for an extended period (at least three[6] to six months, up to years, decades or indefinitely[7]) after ceasing to take the drug. Although the condition is most commonly associated with SRIs, similar or identical syndromes have also been reported after discontinuation of a variety of non-SRI drugs.[8]
| Post-SSRI sexual dysfunction | |
|---|---|
| Other names | Post-SSRI syndrome |
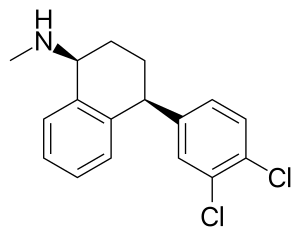 | |
| Chemical structure of sertraline (Zoloft), an SSRI that is reported to cause PSSD in some users | |
| Symptoms | Sexual dysfunction (e.g. erectile dysfunction, loss of vaginal lubrication, anorgasmia, reduced libido), cognitive dysfunction (e.g. anhedonia, emotional blunting, memory loss, shortened attention span) |
| Duration | Months to years after stopping an SRI |
| Causes | Serotonin reuptake inhibitor (SRI) medications, most commonly selective serotonin reuptake inhibitors (SSRIs) |
| Risk factors | Unknown due to lack of data |
| Diagnostic method | Sexual dysfunction symptoms that persist longer than 3-6 months after stopping an SSRI, in the absence of other conditions/medications that could account for symptoms |
| Treatment | No known reliable treatment |
| Frequency | Unknown due to lack of data |
First reported in the medical literature in 2006,[9][10] PSSD remains poorly-understood, with its biological mechanism, risk factors and frequency of occurrence being unknown. The reported symptoms of PSSD commonly include reduced sexual desire or arousal, erectile dysfunction in males or loss of vaginal lubrication in females, difficulty having an orgasm or loss of pleasurable sensation associated with orgasm, and a reduction or loss of sensitivity in the genitals or other erogenous zones. Additional non-sexual symptoms are also commonly described, including emotional numbing, anhedonia, depersonalization or derealization, and cognitive impairment.[6][11] It is considered a distinct clinical pathology from antidepressant discontinuation syndrome, post-acute withdrawal syndrome, and major depressive disorder.[11][12]
There is currently no known reliable treatment for PSSD.[12] To date, the mechanism by which SRIs may induce PSSD is unknown,[5][12][11] as is the exact mechanism by which SRIs induce sexual dysfunction in many patients actively taking the drugs.[13] The symptoms of PSSD are largely shared with post-finasteride syndrome (PFS) and post-retinoid sexual dysfunction/post-Accutane syndrome (PRSD/PAS), two other poorly-understood iatrogenic conditions which have been suggested to share a common etiology with PSSD despite being caused by different types of medication.[14]
Symptoms and diagnosis
According to diagnostic criteria submitted by David Healy et al. in 2022, a diagnosis of PSSD requires that the subject has previously taken an SSRI or other SRI, and has experienced new (i.e. not present before starting the SRI) symptoms of sexual dysfunction for at least three months after the last dose of the SRI;[6] others have proposed a timeline of at least six months of sexual dysfunction symptoms after cessation of the SRI. Other potential causes of sexual dysfunction should be considered and excluded before a diagnosis is made.[12][6]
The following symptoms have been reported in association with PSSD:
- Erectile dysfunction[11][12]
- Loss of vaginal lubrication[12]
- Genital numbness[15]/reduced genital sensitivity (genital anesthesia)[12]
- Inability to achieve orgasm (anorgasmia)[16][17][18][7][5][19][11]
- Reduced pleasure associated with orgasm[11][20][12]
- Premature ejaculation[12]
- Reduced sexual desire/libido[20][12]
- Reduced ability to become sexually aroused[20]
- Decreased penile or testicular size[12]
- Changes in menstrual cycle[12]
- Testicular pain[12]
- Decreased seminal volume and/or quality[6][12]
- Anhedonia[11][6]
- Emotional blunting/numbing[6][11]
- Difficulty thinking or concentrating ("brain fog")[6]
- Issues with memory and recall[17][21]
- Depersonalization[6]
- Derealization[4][22]
- Pelvic floor dysfunction[6]
- Interstitial cystitis/painful bladder syndrome, often diagnosed as recurrent urinary tract infections in females or as recurrent prostatitis in males[6]
In many cases, PSSD sufferers report that their symptoms will transiently improve for short periods (usually no more than one or two days) before returning to their previous state.[10]
Duration of symptoms
The length of time during which PSSD symptoms persist appears to vary among patients, with some cases resolving in a matter of months and others persisting for years or even decades; one analysis of patient reports in the Netherlands submitted between 1992 and 2021 listed a case which had reportedly persisted for 23 years.[7]
Acknowledgements and warnings issued
The UK's Medicines and Healthcare products Regulatory Agency (MHRA) has issued informational leaflets and/or labels containing warnings about post-discontinuation sexual side effects for Sertraline (Zoloft),[23][24] Citalopram (Cipramil),[25][26][27] Paroxetine (Paxil/Seroxat),[28][29] and Fluvoxamine (Luvox/Faverin).[30][31] The FDA has issued a leaflet for Fluoxetine (Prozac/Sarafem) containing similar warnings.[32]
Warnings about post-discontinuation sexual dysfunction associated with SSRIs can be found in the British National Formulary (BNF),[33][34][35][36][37][38] the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders (DSM-5),[39] the Textbook of Rare Sexual Medicine Conditions,[40][41] and the textbook Psychiatry and Sexual Medicine: A Comprehensive Guide for Clinical Practitioners.[42][43]
On the 11th of June 2019, the Pharmacovigilance Risk Assessment Committee of the European Medicines Agency concluded that a possible relationship exists between SSRI use and persistent sexual dysfunction after cessation of use. The committee concluded that a warning should be added to the label of SSRIs and SNRIs regarding this possible risk.[44][45] The Hong Kong Department of Health,[46][47] Health Canada[45][48] and the NHS[49] have also issued warnings about PSSD.
Prevalence and risk
Medications known to cause PSSD
Although PSSD is most commonly reported following cessation of SSRIs, cases have also been reported following the use of serotonin-norepinephrine reuptake inhibitors (SNRIs), SRI tricyclic antidepressants, atypical antidepressants such as mirtazapine, SRI antihistamines, tetracycline antibiotics such as doxycycline, analgesics such as tramadol, and antipsychotics such as aripriprazole.[6][18][8]
Frequency of PSSD
Due to a lack of large-scale, well-controlled studies, there are currently no reliable estimates of how many individuals worldwide suffer from PSSD, nor what fraction of SRI users develop PSSD after stopping the drug. The condition has been suggested to be under-reported.[12]
Data released in 2021 under the UK's Freedom of Information Act by the Medicines and Healthcare Products Regulatory Agency showed that in a total of 1654 cases of adverse effects from SSRIs, in 1069 cases the reaction did not continue after the drug was withdrawn, in 225 cases the reaction continued after the drug was withdrawn with the recovery time being unknown, and in 144 cases the reaction continued after the drug was withdrawn and the recovery time was known.[50]
A retrospective review published in The Journal of Urology in 2020 stated that between 2009 and 2019, 4% of the male patients whose charts were assessed in the review (43 patients total) met the criteria for PSSD, having displayed sexual dysfunction symptoms for longer than 6 months after stopping an SSRI.[51] In 2023, a retrospective analysis of patient records across 19 years at Clalit Health Services, the largest HMO in Israel, found that 0.46% (1 in 216) of surveyed patients who had been treated with serotonergic antidepressants developed symptoms of erectile dysfunction consistent with PSSD.[52]
In 2019, a study published by the Utrecht University (NL) on a sample of healthy adults, investigated the prevalence of persistent sexual dysfunction after the discontinuation of SSRIs antidepressant, focusing on a wider range of symptoms than other studies. The results showed that 52.6% of participants suffered from persisting sexual dysfunction while 26.3% suffered from genital anesthesia and/ or nipple insensitivity. Persisting sexual dysfunction was shown to negatively influence the perceived quality of life.[53] These data are consistent with the findings of previous reports that reported persistent changes in sexual functioning after a treatment with SSRIs.[54][55]
SRI dosage response and other risk factors
It is unknown whether there is a relationship between the amount of time a person has been taking an SRI and the likelihood of developing PSSD. In one case study published in 2006, persistent sexual dysfunction was evident for seven years after taking an SRI for a period of only five weeks;[9] there have been reports of cases developing after only a few, or even single doses of an SRI.[12]
Adolescence, childhood, and development
Several studies in both humans and animals have suggested that use of SSRIs at an early age may increase the likelihood of asexuality during later development. A 2020 study in which 610 young adult individuals were surveyed found that childhood SSRI use among female participants was strongly correlated with reduced sexual desire and activity; childhood SSRI use among male participants was correlated with reduced frequency of partnered sexual activity as an adult.[56] There are reports of sexual dysfunction, often enduring, caused by SSRIs in adolescents, but the incidence of long-term consequences of adolescent SSRI exposure are unknown, possibly due to a lack of baseline sexual experience for comparison.[57] Animal studies on the long-term effects of adolescent SSRI administration have indicated that SSRIs may produce deficits in sexual functioning that persist well after cessation of SSRI treatment and into adulthood, including significantly reduced ejaculation frequency and increased mount latency.[58][59][60]
Hypothesized etiologies
To date, the biological mechanism responsible for causing PSSD, as well as why the symptoms persist long after discontinuation of SSRIs/SNRIs, remain unknown. Researchers have formulated several hypotheses as to the cause of PSSD, starting with the already known molecular mechanisms underlying sexual side effects during SSRI/SNRI treatment. These include increased serotonin, dopaminergic inhibition, inhibition of nitric oxide synthase, increased prolactin, reduced testosterone levels, blockade of cholinergic and alpha-1 adrenergic receptors, effects on proopiomelanocortin and melanocortin, and dysregulation of the hypothalamic–pituitary–gonadal axis.[19][61]
Furthermore, neurochemical changes related to sexual dysfunction during the use of antidepressants have been noted in the peripheral nervous system. This is noteworthy because 95% of serotonin receptors are located outside the brain.[62] It has therefore been hypothesized that PSSD may involve serotonin levels in peripheral nerves.[61]
Hypotheses that attempt to explain the long-term persistence of PSSD symptoms have suggested that epigenetics,[63][64] peripheral sensory neuropathy at the expense of ion channels,[65] bioelectric changes in the resting potential of cells,[66] persistent alteration of neurosteroid levels in the central and peripheral nervous system, and alterations to the gut microbiome[67][68][14] may be potential causative or contributing factors.
A 2020 study found a high incidence of penile tissue fibrosis in a sample of 43 male patients with PSSD, especially among those who had severe erectile dysfunction.[51]
Treatment
There is as yet no established treatment for PSSD. In an unknown fraction of cases, symptoms are reported to resolve spontaneously with time,[10] but the duration of symptoms appears to vary widely among patients. Many anecdotal self-reports exist in which various approaches, ranging from pharmacological or psychiatric treatments to dietary or lifestyle changes, allegedly correlate with improvement in PSSD symptoms, but these results have not been independently verified or replicated. Several studies have been conducted which attempt to identify viable treatments for PSSD,[17][18][65] but in general these have suffered from a small sample size and lack of controls, limiting their informative utility.
Societal impact and support communities
Since 2006,[69] a number of news articles have been published by various outlets on the subject of PSSD.[70][71][72][73][74][75][76][77]
Several online support communities for PSSD exist, including the PSSD Network,[78] PSSD forum,[79] and the PSSD subreddit (r/PSSD on Reddit).
In December 2020, patients in the community started a fundraising campaign to enable the continuation of research into the aetiology of PSSD.[80]
On 21 June 2022, the advocacy organization RxISK began a research fund to support and stimulate interest in PSSD research;[81] the group has also offered a prize of $100,000 USD to anyone who can identify a reliable cure for persistent sexual side effects after stopping antidepressants, finasteride (Propecia), or isotretinoin (Accutane).[82]
In June 2023, the BBC documentary series Panorama released an episode on antidepressant use, titled "The Antidepressant Story". This episode contained a segment discussing PSSD, which included testimonies from PSSD sufferers and an interview with David Healy.[83]
Several medical practitioners, including David Healy[84] and Josef Witt-Doerring,[85] have made efforts to increase awareness of PSSD.
Similar conditions
PSSD is one of several known iatrogenic syndromes characterized by persistent sexual dysfunction after stopping a medication; others include:[6]
- Post-Finasteride Syndrome (PFS), a condition affecting some individuals treated with the hair-loss drug finasteride (Propecia)[14][86]
- Post-Retinoid Sexual Dysfunction (PRSD) or Post-Accutane Syndrome (PAS), a condition affecting some individuals treated with the acne medication isotretinoin (Accutane)[6]
- Hard Flaccid Syndrome (HFS), which has been reported to occur following the use of bremelanotide[87]
- Persistent Genital Arousal Disorder (PGAD), which has been reported to occur in some female patients either while taking or after stopping SSRIs[88][89]
In 2014, a review of 120 reports submitted to RxISK from more than 20 countries concluded that PSSD, PFS and PRSD/PAS exhibit extensively overlapping symptom profiles.[90]
The drug 3,4-methylenedioxymethamphetamine (MDMA), which acts to stimulate the release and inhibit the reuptake of serotonin, can in some cases produce adverse effects that persist long after the drug has been withdrawn, including neurocognitive impairments such as mood disorders[91] and sexual dysfunction.[15] The mechanism behind MDMA neurotoxicity is not fully understood,[91] but a similar mechanism has been suggested to potentially play a role in PSSD.[15]
References
- Bahrick AS (5 May 2008). "Persistence of Sexual Dysfunction Side Effects after Discontinuation of Antidepressant Medications: Emerging Evidence". The Open Psychology Journal. 1 (1): 42–50. doi:10.2174/1874350100801010042.
- Jannini TB, Lorenzo GD, Bianciardi E, Niolu C, Toscano M, Ciocca G, et al. (2022). "Off-label Uses of Selective Serotonin Reuptake Inhibitors (SSRIs)". Current Neuropharmacology. 20 (4): 693–712. doi:10.2174/1570159x19666210517150418. PMC 9878961. PMID 33998993. S2CID 234745872.
- Waldinger MD (1 January 2015). "Chapter 27 - Psychiatric disorders and sexual dysfunction". In Vodušek DB, Boller F (eds.). Handbook of Clinical Neurology. Neurology of Sexual and Bladder Disorders. Vol. 130. Elsevier. pp. 469–489. doi:10.1016/B978-0-444-63247-0.00027-4. ISBN 9780444632470. PMID 26003261. Retrieved 6 January 2023.
- Gründer G (15 November 2021). Psychopharmaka absetzen? Warum, wann und wie? (in German). Elsevier Health Sciences. ISBN 978-3-437-06383-1.
- Reisman Y (October 2017). "Sexual Consequences of Post-SSRI Syndrome". Sexual Medicine Reviews. 5 (4): 429–433. doi:10.1016/j.sxmr.2017.05.002. PMID 28642048.
- Healy D, Bahrick A, Bak M, Barbato A, Calabrò RS, Chubak BM, et al. (1 January 2022). "Diagnostic criteria for enduring sexual dysfunction after treatment with antidepressants, finasteride and isotretinoin". The International Journal of Risk & Safety in Medicine. 33 (1): 65–76. doi:10.3233/JRS-210023. PMC 8925105. PMID 34719438.
- Chinchilla Alfaro K, van Hunsel F, Ekhart C (April 2022). "Persistent sexual dysfunction after SSRI withdrawal: a scoping review and presentation of 86 cases from the Netherlands". Expert Opinion on Drug Safety. 21 (4): 553–561. doi:10.1080/14740338.2022.2007883. PMID 34791958. S2CID 244347777.
- Healy D, Bahrick A, Bak M, Barbato A, Calabrò RS, Chubak BM, et al. (22 February 2022). "Diagnostic criteria for enduring sexual dysfunction after treatment with antidepressants, finasteride and isotretinoin". The International Journal of Risk & Safety in Medicine. 33 (1): 65–76. doi:10.3233/JRS-210023. PMC 8925105. PMID 34719438.
- Csoka AB, Shipko S (2006). "Persistent sexual side effects after SSRI discontinuation". Psychotherapy and Psychosomatics. 75 (3): 187–188. doi:10.1159/000091777. PMID 16636635. S2CID 33448116.
- Healy D (September 2019). "Post-SSRI sexual dysfunction & other enduring sexual dysfunctions". Epidemiology and Psychiatric Sciences. 29: e55. doi:10.1017/S2045796019000519. PMC 8061302. PMID 31543091.
- Peleg LC, Rabinovitch D, Lavie Y, Rabbie DM, Horowitz I, Fruchter E, Gruenwald I (January 2022). "Post-SSRI Sexual Dysfunction (PSSD): Biological Plausibility, Symptoms, Diagnosis, and Presumed Risk Factors". Sexual Medicine Reviews. 10 (1): 91–98. doi:10.1016/j.sxmr.2021.07.001. PMID 34627736. S2CID 238580777.
- Bala A, Nguyen HM, Hellstrom WJ (January 2018). "Post-SSRI Sexual Dysfunction: A Literature Review". Sexual Medicine Reviews. 6 (1): 29–34. doi:10.1016/j.sxmr.2017.07.002. PMID 28778697.
There is still no definitive treatment for PSSD. Low-power laser irradiation and phototherapy have shown some promising results.
- Rosen RC, Lane RM, Menza M (February 1999). "Effects of SSRIs on sexual function: a critical review". Journal of Clinical Psychopharmacology. 19 (1): 67–85. doi:10.1097/00004714-199902000-00013. PMID 9934946.
- Giatti S, Diviccaro S, Panzica G, Melcangi RC (August 2018). "Post-finasteride syndrome and post-SSRI sexual dysfunction: two sides of the same coin?". Endocrine. 61 (2): 180–193. doi:10.1007/s12020-018-1593-5. PMID 29675596. S2CID 4974636.
- Ben-Sheetrit J, Aizenberg D, Csoka AB, Weizman A, Hermesh H (June 2015). "Post-SSRI Sexual Dysfunction: Clinical Characterization and Preliminary Assessment of Contributory Factors and Dose-Response Relationship". Journal of Clinical Psychopharmacology. 35 (3): 273–278. doi:10.1097/JCP.0000000000000300. PMID 25815755. S2CID 2523437.
- Velez D, Ohlander S (September 2021). "Medical therapies causing iatrogenic male infertility". Fertility and Sterility. 116 (3): 618–624. doi:10.1016/j.fertnstert.2021.07.1202. PMID 34462096.
- Reisman Y, Jannini TB, Jannini EA (1 August 2022). "Post-Selective Serotonin Reuptake Inhibitor Sexual Dysfunctions (PSSD): Clinical Experience with a Multimodal Approach". Journal of Men's Health. 18 (8): 165. doi:10.31083/j.jomh1808165. ISSN 1875-6867. S2CID 251371080.
- De Luca R, Bonanno M, Manuli A, Calabrò RS (September 2022). "Cutting the First Turf to Heal Post-SSRI Sexual Dysfunction: A Male Retrospective Cohort Study". Medicines. 9 (9): 45. doi:10.3390/medicines9090045. PMC 9503765. PMID 36135826.
- Bala A, Nguyen HM, Hellstrom WJ (January 2018). "Post-SSRI Sexual Dysfunction: A Literature Review". Sexual Medicine Reviews. 6 (1): 29–34. doi:10.1016/j.sxmr.2017.07.002. PMID 28778697.
- Reisman Y (February 2020). "Post-SSRI sexual dysfunction". BMJ. 368: m754. doi:10.1136/bmj.m754. PMID 32107204. S2CID 211557435.
- "Post SSRI/SNRI Sexual Dysfunction (PSSD)". Sex[M]ed. 15 November 2021. Retrieved 18 January 2023.
- Healy D (April 2020). "Antidepressants and sexual dysfunction: a history". Journal of the Royal Society of Medicine. 113 (4): 133–135. doi:10.1177/0141076819899299. PMC 7160790. PMID 31972096.
- "MHRA Products | Search results". products.mhra.gov.uk. Retrieved 14 December 2022.
- "Package leaflet Information for the patient Sertraline 50 mg Film-coated Tablets Sertraline 100 mg Film-coated Tablets". Archived from the original on 14 December 2022.
- "MHRA Products | Search results". products.mhra.gov.uk. Retrieved 14 December 2022.
- "Citalopram 10 mg, 20 mg & 40 mg Tablets". Medicines and Healthcare products Regulatory Agency (MHRA) products. Archived from the original on 14 December 2022.
- "leaflet". Archived from the original on 14 December 2022.
- "MHRA Products | Search results". products.mhra.gov.uk. Retrieved 14 December 2022.
- "leaflet". Archived from the original on 14 December 2022.
- "MHRA Products | Search results". products.mhra.gov.uk. Retrieved 14 December 2022.
- "Package leaflet: Information for the user". Archived from the original on 14 December 2022.
- "FDA medication leaflet" (PDF). Archived (PDF) from the original on 6 January 2023.
- "Sertraline". DRUGS BNF NICE. Retrieved 29 January 2023.
- "Citalopram DRUGS BNF NICE". Retrieved 29 January 2023.
- "Fluoxetine". DRUGS BNF NICE. Retrieved 29 January 2023.
- "Fluvoxamine DRUGS". BNF NICE. Retrieved 29 January 2023.
- "Escitalopram". DRUGS BNF NICE. Retrieved 29 January 2023.
- "Paroxetine". DRUGS BNF NICE. Retrieved 29 January 2023.
- Diagnostic and Statistical Manual of Mental Disorders. USA: American Psychiatric Association. 2013. p. 449.
In some cases, serotonin reuptake inhibitor induced sexual dysfunction may persist after the agent is discontinued
- Reisman Y, Lowenstein L, Tripodi F, eds. (2022). Textbook of Rare Sexual Medicine Conditions. doi:10.1007/978-3-030-98263-8. ISBN 978-3-030-98262-1. S2CID 248991620.
- Reisman Y, Pfaus JG, Lowenstein L (2022). "Post-SSRI Sexual Dysfunction (PSSD)". In Reisman Y, Lowenstein L, Tripodi F (eds.). Textbook of Rare Sexual Medicine Conditions. Cham: Springer International Publishing. pp. 51–63. doi:10.1007/978-3-030-98263-8_5. ISBN 978-3-030-98263-8.
- Lew-Starowicz M, Giraldi A, Krüger TH, eds. (2021). Psychiatry and Sexual Medicine. doi:10.1007/978-3-030-52298-8. ISBN 978-3-030-52297-1. S2CID 221400846.
- "Psychiatry and Sexual Medicine". Canadian PSSD Society. Retrieved 10 January 2023.
- Pharmacovigilance Risk Assessment Committee (PRAC). "Minutes of PRAC meeting on 13-16 May 2019" (PDF). European Medicines Agency. p. 25.
- "Summary Safety Review – Selective Serotonin Reuptake Inhibitors (SSRIs) and Serotonin-norepinephrine Reuptake Inhibitors (SNRIs) – Assessing the Potential Risk of Sexual Dysfunction despite Treatment Discontinuation". 6 January 2021. Archived from the original on 17 January 2021.
- "HongKong Warning". 7 January 2021. Archived from the original on 12 December 2022.
- "Hong Kong announcement". Canadian PSSD Society. Retrieved 13 December 2022.
- "Health Canada warns about Persistent Sexual Dysfunction after SSRIs & SNRIs | RxISK". rxisk.org. Retrieved 13 December 2022.
- "Side effects of escitalopram". nhs.uk. 25 February 2022. Retrieved 26 March 2023.
- "Freedom of Information request on adverse sexual dysfunction reactions to SSRI use (FOI 21-232)". GOV.UK. Archived from the original on 6 January 2023. Retrieved 20 December 2022.
- Waraich A, Clemons C, Ramirez R, Yih J, Goldstein S, Goldstein I (April 2020). "Mp78-15 post-ssri sexual dysfunction (pssd): ten year retrospective chart review". Journal of Urology. 203 (Supplement 4): e1179. doi:10.1097/JU.0000000000000964.015. S2CID 218960429.
- Ben-Sheetrit J, Hermon Y, Birkenfeld S, Gutman Y, Csoka AB, Toren P (April 2023). "Estimating the risk of irreversible post-SSRI sexual dysfunction (PSSD) due to serotonergic antidepressants". Annals of General Psychiatry. 22 (1): 15. doi:10.1186/s12991-023-00447-0. PMC 10122283. PMID 37085865.
- Lüning C (2019). Life after antidepressants: Does persisting sexual dysfunction influence quality of life? (Master Thesis thesis).
- Montejo AL, Llorca G, Izquierdo JA, Carrasco JL, Daniel E, Pérez-Sola V, et al. (1999). "[Sexual dysfunction with antidepressive agents. Effect of the change to amineptine in patients with sexual dysfunction secondary to SSRI]". Actas Españolas de Psiquiatría. 27 (1): 23–34. PMID 10380144.
- Safarinejad MR, Hosseini SY (March 2006). "Safety and efficacy of citalopram in the treatment of premature ejaculation: a double-blind placebo-controlled, fixed dose, randomized study". International Journal of Impotence Research. 18 (2): 164–169. doi:10.1038/sj.ijir.3901384. PMID 16107866. S2CID 30773321.
- Lorenz TK (March 2020). "Antidepressant Use During Development May Impair Women's Sexual Desire in Adulthood". The Journal of Sexual Medicine. 17 (3): 470–476. doi:10.1016/j.jsxm.2019.12.012. PMC 7197954. PMID 31937517.
- Scharko AM (September 2004). "Selective serotonin reuptake inhibitor-induced sexual dysfunction in adolescents: a review". Journal of the American Academy of Child and Adolescent Psychiatry. 43 (9): 1071–1079. doi:10.1097/01.chi.0000131135.70992.58. PMID 15322410.
- Iñiguez SD, Warren BL, Bolaños-Guzmán CA (June 2010). "Short- and long-term functional consequences of fluoxetine exposure during adolescence in male rats". Biological Psychiatry. 67 (11): 1057–1066. doi:10.1016/j.biopsych.2009.12.033. PMC 2868075. PMID 20172503.
- Coskuner ER, Culha MG, Ozkan B, Kaleagasi EO (April 2018). "Post-SSRI Sexual Dysfunction: Preclinical to Clinical. Is It Fact or Fiction?". Sexual Medicine Reviews. 6 (2): 217–223. doi:10.1016/j.sxmr.2017.11.004. PMID 29463440.
- de Jong TR, Snaphaan LJ, Pattij T, Veening JG, Waldinger MD, Cools AR, Olivier B (January 2006). "Effects of chronic treatment with fluvoxamine and paroxetine during adolescence on serotonin-related behavior in adult male rats". European Neuropsychopharmacology. 16 (1): 39–48. doi:10.1016/j.euroneuro.2005.06.004. hdl:1874/19743. PMID 16107310. S2CID 21978633.
- Csoka AB, Bahrick A, Mehtonen OP (January 2008). "Persistent sexual dysfunction after discontinuation of selective serotonin reuptake inhibitors". The Journal of Sexual Medicine. 5 (1): 227–233. doi:10.1111/j.1743-6109.2007.00630.x. PMID 18173768.
- Frohlich PF, Meston CM (1 November 2000). "Evidence that serotonin affects female sexual functioning via peripheral mechanisms". Physiology & Behavior. 71 (3–4): 383–393. doi:10.1016/S0031-9384(00)00344-9. PMID 11150571. S2CID 11053532.
- Kanherkar RR, Getachew B, Ben-Sheetrit J, Varma S, Heinbockel T, Tizabi Y, Csoka AB (25 July 2018). "The Effect of Citalopram on Genome-Wide DNA Methylation of Human Cells". International Journal of Genomics. 2018: 8929057. doi:10.1155/2018/8929057. PMC 6083487. PMID 30148158.
- Csoka AB, Szyf M (November 2009). "Epigenetic side-effects of common pharmaceuticals: a potential new field in medicine and pharmacology". Medical Hypotheses. 73 (5): 770–780. doi:10.1016/j.mehy.2008.10.039. PMID 19501473.
- Waldinger MD, van Coevorden RS, Schweitzer DH, Georgiadis J (April 2015). "Penile anesthesia in Post SSRI Sexual Dysfunction (PSSD) responds to low-power laser irradiation: a case study and hypothesis about the role of transient receptor potential (TRP) ion channels". European Journal of Pharmacology. Mood disorders-preclinical, clinical and translational aspects. 753: 263–268. doi:10.1016/j.ejphar.2014.11.031. PMID 25483212.
- Healy D, LaPalme J, Levin M (March 2020). "Post-SSRI Sexual Dysfunction: A Bioelectric Mechanism?". Bioelectricity. 2 (1): 7–13. doi:10.1089/bioe.2019.0010. PMC 8370302. PMID 34471832.
- Diviccaro S, Giatti S, Cioffi L, Falvo E, Piazza R, Caruso D, Melcangi RC (September 2022). "Paroxetine effects in adult male rat colon: Focus on gut steroidogenesis and microbiota". Psychoneuroendocrinology. 143: 105828. doi:10.1016/j.psyneuen.2022.105828. PMID 35700562. S2CID 249525679.
- Giatti S, Diviccaro S, Cioffi L, Falvo E, Caruso D, Melcangi RC (October 2021). "Effects of paroxetine treatment and its withdrawal on neurosteroidogenesis". Psychoneuroendocrinology. 132: 105364. doi:10.1016/j.psyneuen.2021.105364. hdl:2434/901757. PMID 34325207. S2CID 236165173.
- "PSSD in the Media". UK PSSD Association. Retrieved 18 January 2023.
- Baskerville K (1 December 2022). "What is post-SSRI Sexual Dysfunction (PSSD) and what do I need to know about it?". Mashable. Retrieved 16 December 2022.
- Brown D (3 November 2018). "Antidepressants were supposed to help me but they ended up making me impotent". Metro. Retrieved 27 December 2022.
- "For Some People, the Sexual Side Effects of SSRIs Never Go Away". MEL Magazine. 30 June 2022. Retrieved 27 December 2022.
- Wyton M (2 November 2021). "'Something So Sacred Has Been Taken Away from Me'". The Tyee. Retrieved 10 January 2023.
- ""Despair takes a young man's life"". Canadian PSSD Society. Retrieved 10 January 2023.
- "I Started Taking Zoloft Five Years Ago. I Haven't Felt Sexual Sensation Since". Narratively. 6 September 2016. Retrieved 18 January 2023.
- "Disfunzione sessuale persistente dopo terapia anti-depressiva - Quotidiano Sanità". www.quotidianosanita.it. Retrieved 18 January 2023.
- Simon (23 May 2023). "Antidepressants have destroyed my sexual function and range of emotions". Mad in the UK. Retrieved 6 June 2023.
- "PSSD Network". PSSD Network. Retrieved 21 May 2023.
- "PSSD Forum - Index page". www.pssdforum.org. Retrieved 21 May 2023.
- https://www.pssdnetwork.org/donate
- "Post-SSRI Sexual Dysfunction (PSSD) Research Fund | RxISK". rxisk.org. Retrieved 3 December 2022.
- "RxISK Prize: Sexual problems after antidepressants, finasteride & isotretinoin | RxISK". rxisk.org. Retrieved 17 December 2022.
- "BBC Panorama: The Antidepressant Story". PSSD Network. Retrieved 23 June 2023.
- Post-SSRI Sexual Dysfunction (PSSD) - Professor David Healy, retrieved 6 May 2023
- Interview with Carlton Ellison - Post-SSRI Sexual Dysfunction, retrieved 6 May 2023
- Diviccaro S, Melcangi RC, Giatti S (May 2020). "Post-finasteride syndrome: An emerging clinical problem". Neurobiology of Stress. 12: 100209. doi:10.1016/j.ynstr.2019.100209. PMC 7231981. PMID 32435662.
- Abdessater M, Kanbar A, Akakpo W, Beley S (4 June 2020). "Hard flaccid syndrome: state of current knowledge". Basic and Clinical Andrology. 30: 7. doi:10.1186/s12610-020-00105-5. PMC 7271516. PMID 32518654.
- Leiblum SR, Goldmeier D (2008). "Persistent genital arousal disorder in women: case reports of association with anti-depressant usage and withdrawal". Journal of Sex & Marital Therapy. 34 (2): 150–159. doi:10.1080/00926230701636205. PMID 18224549. S2CID 11186202.
- Kruger TH, Schippert C, Meyer B (March 2020). "The Pharmacotherapy of Persistent Genital Arousal Disorder". Current Sexual Health Reports. 12 (1): 34–39. doi:10.1007/s11930-020-00240-0. ISSN 1548-3592. S2CID 210716154.
- Hogan C, Le Noury J, Healy D, Mangin D (1 January 2014). "One hundred and twenty cases of enduring sexual dysfunction following treatment". The International Journal of Risk & Safety in Medicine. 26 (2): 109–116. doi:10.3233/JRS-140617. PMID 24902508.
- Sarkar S, Schmued L (August 2010). "Neurotoxicity of ecstasy (MDMA): an overview". Current Pharmaceutical Biotechnology. 11 (5): 460–469. doi:10.2174/138920110791591490. PMID 20420572.